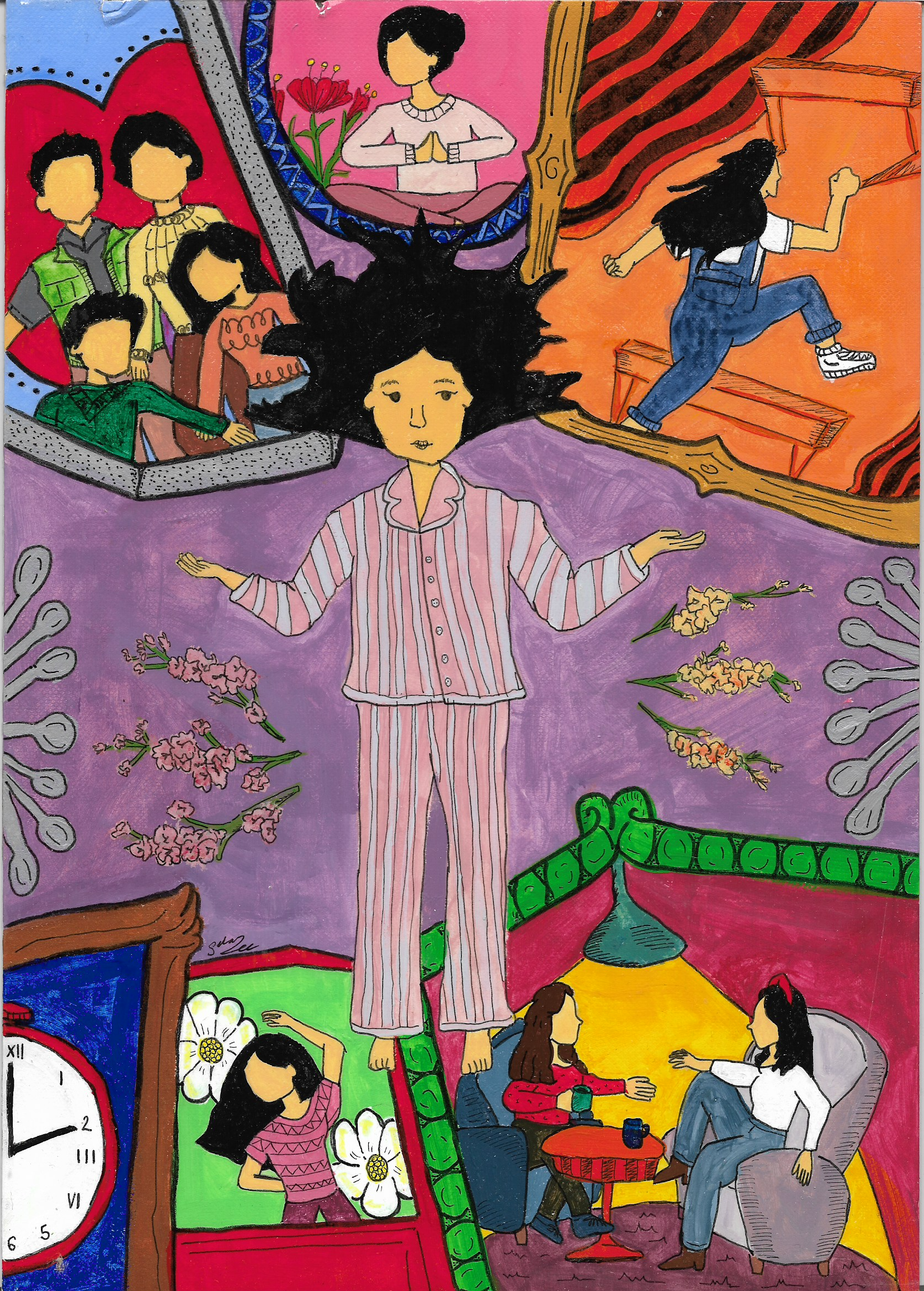
Why Finding Your People Matters
By Maria Rouse
It took me nearly 15 years to begin finding community as someone with inflammatory bowel disease. It was a very lonely 15 years.
I try not to be so hard on myself, since I was first diagnosed with IBD when I was 10. There is not much in the way of accessible peer support for youth with IBD, especially at that young of an age. It was not an option I ever realized could be possible through my health system, and social media as a platform for peer support was just beginning at that time.
My inability to find community led to a false perception of singular failure. I was the only person my age that I knew with IBD, and consequently internalized ableism spread malignantly within my mind and began marring my conception of myself.
With the stigma associated with IBD, it is also not something you typically share about yourself with other kids on the playground, or even when you’re getting to know people during orientation at college. I have met several friends that I only much later learned had IBD.
Ableism is a key motivating force in keeping us silent from sharing our stories and lived experience with others. Ableism is part and parcel of patriarchy, colonialism, racism, sexism, or most of the negative isms that still permeate society. It encourages us to remain alone in our journeys as chronically ill people.
In a system that often tries to force us to act individualistically and hide our unique qualities for the sake of its imposed and exalted definition of success, building disability community is a light in the darkness. It is in itself an act of resistance and radical vulnerability in a society aims to police abnormality and difference. This can make us believe that our challenges and needs are uniquely too much, when nothing could be further from the truth. Community reminds us of our humanity as chronically ill people.
In any setting, making new connections and friends can be terrifying, particularly if you have felt so alone and different all your life as a person with a chronic illness. It can feel especially vulnerable to join a support group discussing such sensitive topics as disordered eating and body image with a whole new groups of people. But forming community through a group such as CCYAN is so worth any initial awkwardness or difficult topics.
The reality is that peer support is not just about you, although it often is cathartic and restorative to know we are not alone and to learn how others managed the difficulties that IBD created in their lives. Peer support is also an act of advocacy, allowing disabled and/or chronically people to take up space when so often our voices are not heard. Building community is an act of advocacy for yourself and also others who may still face barriers in sharing their experiences.
In short, don’t wait years to engage with peers who have IBD. Make time for that peer support group meeting, attend that advocacy event, or connect with peers over Instagram. There are typically more obstacles for chronically ill people to engage with peers, whether that is being immunocompromised or having limited spoons or energy. However, engaging with other IBDers in whatever format is accessible to you is well worth the effort. Life is truly all about connections, and the ones you make with those who have very similar experiences as you can be some of the strongest bonds you will experience. You never know what can come out of it, and how the world could be changed for the better.
Featured photo by Darrel Und from Pexels.