By Nikhil Jayswal
Disclaimer: The views presented in this article are entirely my own.
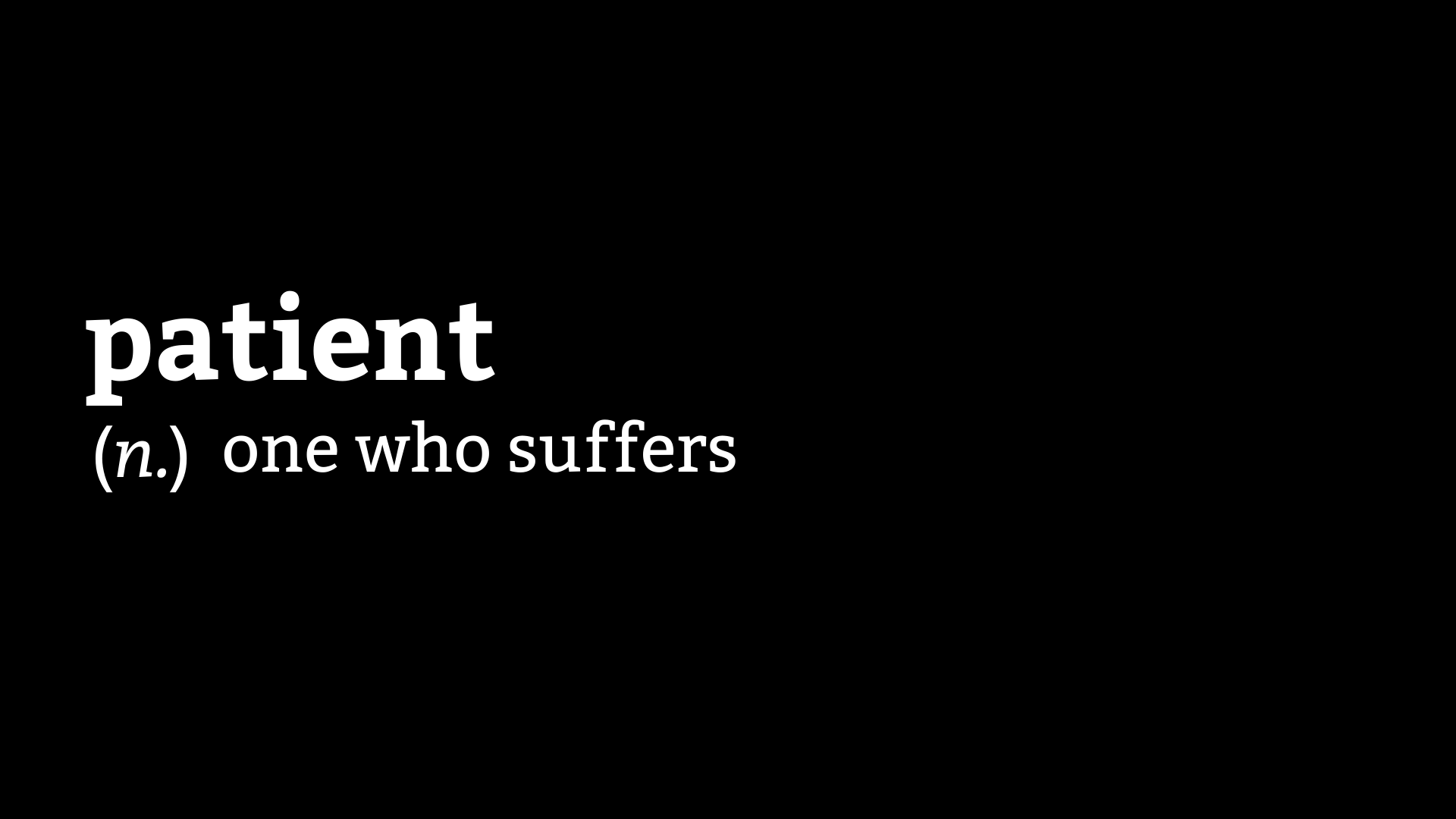
A couple of years ago, I stumbled upon the original definition of a patient - “one who suffers”. The word comes from the Latin word patiens, which is the present participle of the deponent verb, patior, which means “I am suffering.”
This definition, for some reason, is stuck in my mind, and I can’t help but ponder over it in many different ways whenever I come across it. Everything that I have ever experienced while navigating the healthcare system, makes me realize that I’m a patient because I’m patient. My virtue is now my label. The very characteristic that can garner someone praise is now a label for an ill person. To me, this contrast feels poetic, ironic, and cruel, all at the same time.
I tend to be very patient unless I’m in pain. I never knew though, that my patience, in essence, is my capacity for suffering. My patience has often been tested to the limits, by the healthcare system in my country. I can understand that the public healthcare system is not equipped to handle the volume of patients that it receives, which leads to delays and substandard care, but the private healthcare system has not been very kind to me either. The private healthcare system unfairly treats patients with weaker socio-economic backgrounds and highly favors the affluent ones. People with affluence and influence rarely respect any rules and often indulge in corrupt, immoral, and unethical practices to hijack the system and get the treatment that they want. This has often caused me much pain. I have struggled to find a hospital bed or a doctor on time, and I have been treated badly by the system because of my inability to afford the treatment I needed to stay alive.
It seems almost futile to me, to speak of these issues, because of a lack of support and the fact that people have accepted these issues. Breaking the rules to deny someone else the care that they might need more urgently is not a matter of concern for most people. In such an environment, only two kinds of people survive - the affluent or the patient. The word “patient”, hence, should be reserved for those who ultimately pay the price of a broken system, being abused further by egocentric people. This system has often made me and my mother weep as we struggled and oftentimes, begged for aid. Be it drugs, insurance, hospital admissions, diagnostics, or appointments, the entire ecosystem feels like one huge paywall.
People struggling with similar conditions are competing against one another to get care. Instead of standing together as a community, we are competing with each other, and the game is of patience. How early can you come to queue up at the OPD (outpatient department) window? How many hours are you willing to wait to see the doctor? However, the ones who win are those who do not play this game and the only thing you can do as you watch them get ahead of you is feel sorry for yourself and be ... patient.
Every time I write a part of my story, I relive a lot of trauma, caused not only by my illness but also by the healthcare system. Aiming to be an advocate amidst such an environment seems to be a foolish undertaking. In this system, money, power, and influence are advocates. I was incredibly lucky to survive. There are some who are trying to do their jobs as rightly as possible in this atmosphere, and it is these people, to whom I owe my life.
Privilege and patience have an inverse relationship. The more privilege you have, the less is the patience you can get away with. I have the privilege of education. I have the privilege of being able to obtain and absorb information on my own. I have the privilege of graduating from one of the best institutes in India. Without all these privileges, I would not be where I am today. These privileges though, are not of much use if you are not a person of importance, or a person of wealth, and are suffering from a severe form of some chronic illness.
These days I stare a lot out of my house to see people taking a walk, some with their pets, kids playing on the street, etc. When I look at them, I feel the same hollowness in my heart that I felt a few years ago, when I looked out of the hospital windows, at the outside world. My home feels like a prison to me now. I cannot step out of my house because people are not wearing masks, even after the fact that three COVID cases have been detected in the neighborhood. The lockdown may be over for other people, but it continues for me. The reason is simple. Even though wearing a mask and social distancing rules are not laws, breaking these rules to deny someone else (in this case, the vulnerable population) the simple pleasure of walking outdoors is not a matter of concern for most people. They’re not patients. I am. I haven’t been able to follow-up with my doctor in six months. I’m buying my ostomy supplies at higher rates than usual. Why? Because I’m a patient, and thus it is my destiny to suffer. Thankfully, I am not in a flare, but many of my friends are, and they are unable to step outside to buy medicines. Why? Because they’re patients too.
Now anytime, someone tells me that I’m a patient man, the irony and cruelty of it dawns upon me. This word often rings and echoes around in my head, and it has been doing so much more these days as I feel trapped and helpless, and at the mercy of the non-patient population. Advocacy, currently in India, has many different dimensions, that are neither pretty nor easy. Similar to the ecosystem that thrives on the patience of the under-privileged, we need an ecosystem of advocates, working in different ways, that can help the actual patients get the care they require and deserve without having to suffer as much as they do currently.
Until that happens, for me, and others like me, even though dictionaries define a patient differently now, the experience of being one still echoes, very loudly, the original definition - “one who suffers”.