“‘Inflammatory bowel disease’ (IBD) sounds like a straightforward term — a disease of inflammation in the bowel. However, the history of IBD reveals a story of a nefariously complex set of idiopathic conditions. IBD defies definition, in part because its pathophysiology is not completely understood. For the same reason and despite substantial advances in research, IBD also defies cure. At best, IBD can be defined as a disease of disruption — disrupted physiology, microbiology, immunology and genetics.”1
Repeatedly, one of the challenges I face in having IBD is being able to effectively communicate the severity and uniqueness of the disease to my friends, broader society, and, at times, even myself. The quoted part above from the paper ‘A tale of two diseases: The history of inflammatory bowel disease’ articulates the complexity and vagueness perfectly.
I distinctly remember a time at school when my understanding of the world shifted from ‘adults know everything and humans have control over everything in this universe,’ to teachers starting to draw lines around exactly what is known to us. What’s left out were things even the biggest scientists who got us to the moon couldn’t decipher. During this mind shift, we learned about the limitless scope of space, the depths of the oceans, the uncertainty of what causes psychopaths, and having no cure for cancerous cells, among other things. I remember the fear but also a naïve invincibility that while these uncertainties exist, they will not be applicable to me or my loved ones. But IBD is unpredictable; it can hit almost anyone, at any age. And all the videos I saw on Facebook celebrating the new reaches of technology in healthcare – like that one video of a microcamera in a dissolvable pill helping doctors to see inside the digestive tract without invasive procedures – were just that, videos of research trials. The reality was always so much more ~simple~ with burdensome invasive procedures, like colonoscopies.
Medications to “manage,” not cure, IBD, are also primitive in the domain of medication, not outstanding. They always come with trade-offs – like ‘Get your colon back, but lose your bones!’ or ‘Stop bleeding, but eat like a garden rabbit for the rest of your life!’ or my personal fav, ‘Manage your illness in the gut, but leave with debilitating fatigue, brain fog, anxiety and depression! Bonus: It’s all in your head, even your doc won’t believe you.’
Living with IBD can be especially difficult due to you having to explain yourself and your situation so much. People may think you have a variant of food poisoning, or you somehow brought it on to yourself with unhealthy eating habits. The stigma about the ways in which IBD exists gives little leeway to understand the severity of it. IBD is both a hidden blessing (maybe blessing is reaching too far) and a curse, as it forces you to learn to be compassionate with yourself (that’s a big part of the closest thing we have to a cure), but shows you the irresponsibility, ignorance and pure apathy of the society around you. With cancer, for example, the pain and trauma are duly acknowledged by society. There is a sense of responsibility the society (whether that’s friends, school, work, strangers) feels to stand in solidarity and be helpful in those moments. In having a chronic illness, granted it is not cancer but still a very traumatic on-going experience, there is no assumed empathy-net provided in those dark moments.
For people like me, with social anxiety and people-pleasing tendencies, explaining the gravity of what you’re going through can be an impossibly difficult task. As I’m nearing my 5th year of having IBD, I confess I still go back and forth between playing it down to not take away from anyone or carrying resentment for people who could not understand in the past. On my best days – enjoying my iced coffee and spicy Indian food - I invalidate myself and ponder, did I really have it that bad or was it all in my head? On my worst days - on my knees, clutching my abdomen or sweating with AC at full blast at 3AM at night - I bitterly revisit the hurtful comments I’ve received over the years. Life has to go on, and in going forward, IBD patients need to build a society that holds space for them.
Here are short notes on how I hold space for myself, and ask people around me to do the same:
1. On Badtameezi
In South Asian families, roles in a family are decided according to the age and relation. For example, a younger person, even if more experienced in a certain field, is not allowed to voice his/her opinion on some subjects; it's called badtameezi.
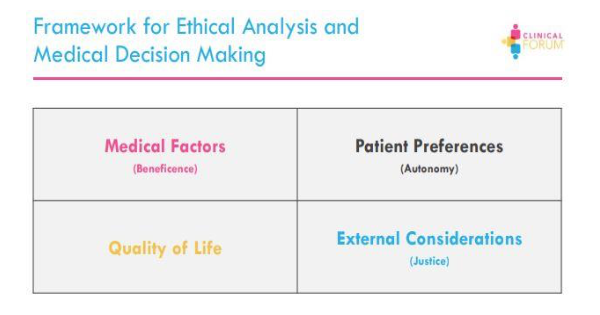
Badtameezi is the South Asian society’s way of manipulating you to exist in a way they deem fit. Practicing privacy, setting boundaries, cutting off from anxiety-inducing family members, and decision autonomy are just a few examples of being a “bad” person. All of the above are obviously necessary for a person with a chronic, stress-related illness, so it becomes important to choose whether you want the badtameez label and health, or tameezdar label and continuously deteriorating health.
2. On Comparison
In the South Asian diaspora, the competitive spirit is a prominent aspect of life. India is the second most populated country on Earth, soon to be first, and resources are low, perhaps that’s why competition is high. While healthy competition is important in bringing out qualities like hard work and ambition, competition about health crosses lines over to absurdity. Yet, this is quite common. A simple “No, it’s not the same,” or “No, I feel like you’re not understanding what I am dealing with,” or “I’m very sorry you had to go through that. My illness however is very different because…” can suffice. If they’re open to it, you can open up about it more.
3. On Self-Invalidation,
It’s useful to journal during flares, not only for the benefit of your mental health, but also to keep track of your feelings on the worst days. To check in with yourself during those times makes it easier to not invalidate your experiences later on. I don’t have the discipline to keep journaling daily, but every time I am in physical pain, I do grab a pen and notebook to jot down my mental state and thoughts, and I refer back to it in times I forget what my experiences have been like. It’s also helpful to engage with a support group; the conversations around other’s experiences with triggers, symptoms, tests, doctor’s visits, work, friends and family can help you understand and navigate your own. Disclaimer though, everyone’s experiences are different in all the dimensions of the disease; your lived experiences will always be unique. Lastly, I like talking to someone who’s seen me at my worst to remind me how it really was, and that it was not all in my head. This could be a close friend or family member.
4. On Unsolicited Comments,
Just call them out on these. It’s 2021, people need to stop commenting on your weight gain/weight loss and any other changes they see in you, irrespective of whether it's due to your illness. A simple but firm statement like “If I need your opinion, I’ll ask for it,” or “I like it this way,” can help establish a boundary.