By Rachael Whittemore
Photo by Sydney Troxell from Pexels
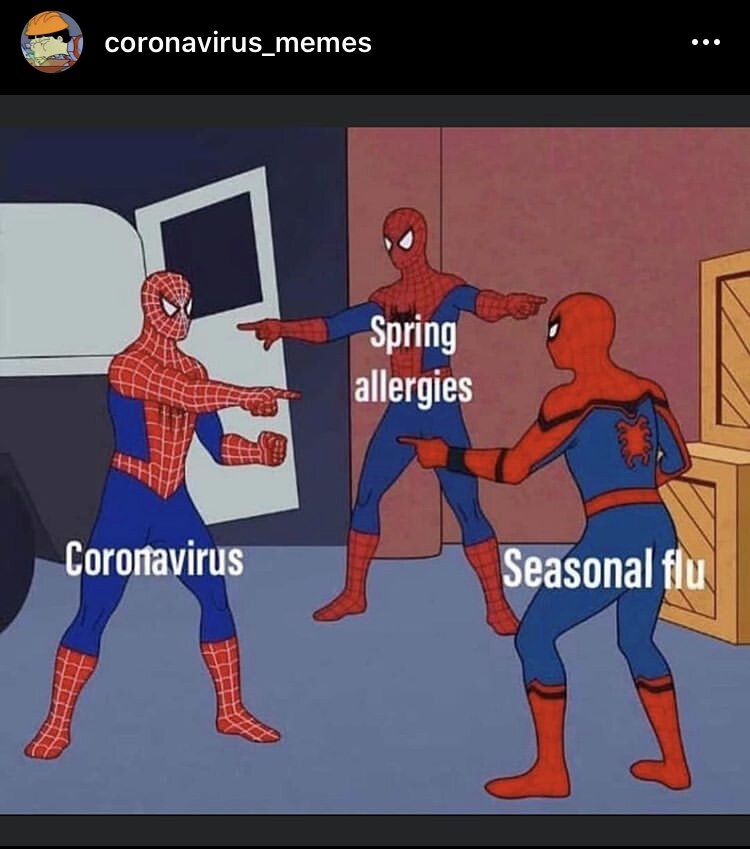
Just like that - we’re well into summer and I almost can’t believe it. Even though it feels like it’s been 10 years since January, I’ve thoroughly enjoyed all the fresh food that comes with this season. The days are longer, the fruit and veggies are ripe and I don’t feel weird about wanting to eat some version of a salad daily. I’m even starting to learn how to garden! (TBD if anything makes it though!) However, as I think about some of my favorite summer foods, it also reminds me that for many of us living with IBD, it’s very possible that our bodies can’t handle some of our favorite foods anymore. After being diagnosed, we probably searched the internet for resources and advice on what to eat, what to avoid, and somewhere along the way we learned that what might work for you might not work for me.
My co-fellow Lucy published a wonderful video last month about how she has learned to thrive with her dietary restrictions and how she’s managed her “break up” with things like dairy. Because having different perspectives can be helpful to all of us living with IBD, writing this was very important to me. I also felt led to write this because if you have met me, you know how much I LOVE food. Cooking food for others and sharing it provides a huge sense of community for my family and me as it does for many others. Certain foods are tied to family by culture, tradition or memories, and it can be a challenge to really stop eating foods that may have been fine before. It also may take time, especially if they were a large part of your diet pre-IBD. Here are some tips for getting away from IBD-problem foods and to find joy in what you can eat and let it nourish your body.
1
Work on accepting that you and this much-loved food and/or food groups just don’t get along.
Living with chronic illness requires us to work through a lot, both physically and mentally. Accepting that we have a lifelong illness is hard in so many ways, especially one that can be unpredictable, embarrassing and frustrating. Accepting that I can no longer eat certain foods I love is difficult too, and we shouldn’t be embarrassed to mourn giving up parts of our pre-IBD life. For me, accepting that something isn’t working for me or my health helps me move forward as I try to live my best life.
2
The short-lived happiness of eating said food(s) is usually not worth what comes later.
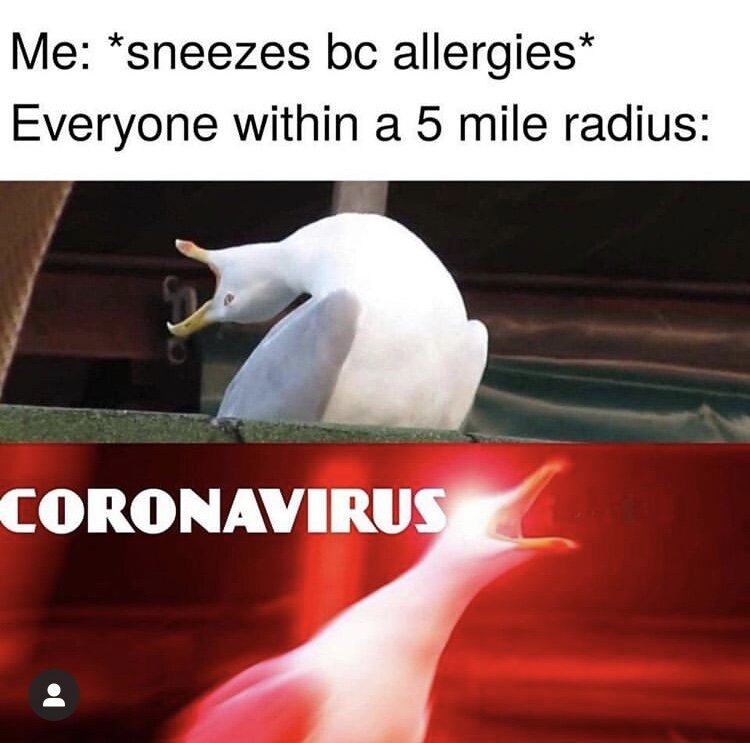
I have personally struggled with this in my journey to give up milk and cheese. I realized that I was likely lactose intolerant in college when I decided to do a month dairy-free. I didn't have IBD yet, but milk and cheese products had always given me issues. There are times when I fooled myself into believing my sensitivity wasn’t that bad, but as I have gone through extended periods of not drinking milk or eating cheese, I feel so much better. No pain, no constipation, less flares and much less bloating or gas.
3
Silver lining? There could be a certain way you can handle said food(s) or food groups.
If you can’t do cow’s cheese, maybe goat cheese works. In my case, I can usually handle regular yogurt without problems, and I will eat small amounts of it with fruit and nut butter to give my body some calcium and ~good bacteria.~ Maybe if certain veggies bother you, try cooking them waaaay down and adding to a favorite dish you like, or cooking them with no seasonings and adding them into something like a smoothie. I love to use baby spinach and greens this way! Other times, you may just decide it’s best to avoid something altogether.
4
Helllooooo substitutes!
The wonderful thing about living in an era where people are more aware of food allergies or sensitivities is that there are more and more substitutes for common food groups that you may need to eliminate. Non-dairy, soy-free, gluten-free, grain-free, nut-free, egg-free, vegetarian, vegan...I know this list goes on and there are many I don’t even know about yet. I have recently tried oat milk and love it because it’s a little creamier and great for coffee and it’s far more sustainable than my usual almond milk. In terms of a vegetarian cheese (no lactose but does have casein), I thought all hope was lost until my roommate introduced me to this almond cheese. It’s my favorite affordable non-lactose cheese and even comes in a pepper jack flavor that’s awesome. Here’s a few links to other things I regularly substitute based on my current diet: my fav oat milk, mac n' cheese, yogurt (with dairy, dairy-free and lactose-free), almond and coconut milk yogurts.
5
Find blogs, Instagram accounts or online recipes that cater to your dietary needs.
This is something else that has been great to have on hand in our digital age. Especially during quarantine, I’ve been trying some new recipes and looking at ways I can eat the things I love without missing the things I had to give up. Sometimes you find some handy, simple tips that you end up carrying with you on your IBD-food journey. Like, who knew that coconut milk and cream created a great base for non-dairy ice cream? If you want a great online account to check out - my co-fellow Rachel Straining has an amazing blog and Instagram: @thenoglutengirl. Give her a follow and check out her amazing yogurt bowls, baked goods and realness about her journey with Crohn’s.
6
Sorry, not sorry.
One of the most important things to do when you’re working on giving up or decreasing consumption of a food is to stick to your guns. It becomes much more challenging when you’re eating out with others and during the holidays. As tempting as it is to eat things you like and not feel like a burden to others, it’s so important that you don’t let this pressure get you down and cave (but I’m definitely guilty of this!). I’ve learned that being real about what I can and can’t eat works out both ways in the end - your body will thank you and you feel confident in the choices you’re making for yourself. You may not realize it, but it empowers your own self-advocacy. :)
These are a few tips just to get you started, but know that all of us living with IBD have gone through this or are still working through it. Sometimes our food tolerances change, and as frustrating as it can be, search for opportunities to try something new or create a new version of something that you miss that still tastes amazing. I empathize with you and understand the frustration of trying to find foods and a diet that works for your needs. IBD makes life harder sometimes, but I know so many people who rise to meet all the challenges they’re faced with. Breaking up with some of your favorite foods may not seem like a big deal, but I’ve been there and I’m still there sometimes. You have no idea how much I wish I could eat chips and queso! Especially if you’re newly diagnosed, take each day at a time and I hope you can find the silver lining one day and laugh at all the times you thought eating *said food* was ok and ended up in bed at 8 pm because of it.