By: Maalvika Bhuvansundar
Hearing the word surgery is enough to give a lot of us nightmares. During my early stages of diagnosis, I was told of a future where surgery might be required, but I never thought such a day would come. Well, looking back at it now, I realize how wrong I was for assuming this. For a lot of us with IBD, surgery might be inevitable. However, there are also a lot of individuals with IBD who might not require surgery and could reach remission with medication and lifestyle changes. It wasn’t the case for me though. After six painful years of being sick, surgery seemed like the most probable solution. Got numerous tests done once again for the 100th time and realized that my intestines were narrowed. The good news was that Remicade was working well for me, and the narrowing was getting better but at a very slow pace! I was given two options, either I could get hemicolectomy surgery done or could rely solely on Remicade which might take longer to ease my symptoms. The following steps helped me make a clear decision:
Make a pros and cons list - having things written out helps make a more objective and rational decision.
Get all the required tests done and always ASK for a copy of your reports.
Always get a second opinion! It’s our body and we have every right to get as many second opinions as we’d like. Don’t let anyone tell you otherwise.
Make a pros and cons list - having things written out helps make a more objective and rational decision.
Ask your doctor every doubt you have regarding the surgery even if it may seem repetitive or irrelevant. It is better to make a decision with all your doubts and concerns answered.
Luckily for me, my aunt and uncle are both doctors, and they assured me that getting this surgery would be the best decision I took, and they were spot on! There are a few things to keep in mind for post-surgery:
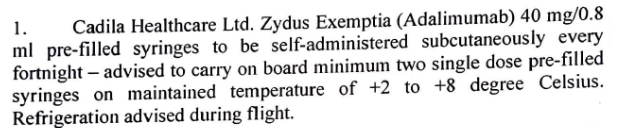
Ensure they have given you the medications required to take at home.
Always write down the instructions given for home care.
Ensure they have given you the medications required to take at home.
Do not leave without the discharge summary!
There are chances of having constipation post-surgery; it is a pretty common side effect. Ask the doctors what to do if this situation pertains to avoid anxiety and stress regarding this once you are back at home.
Do not miss your follow-up appointments!
Thanks to this life-changing surgery, for the first time in six years, I am symptom-free, and though I will always have the scar to remind me of the pain, it also reminds me of the decision that helped me lead a better life. This experience showed me that life could take a different turn unexpectedly. However, the scary choices may sometimes be the best ones we’ve ever taken!